Why this matters in Hong Kong
Hong Kong’s emergency ambulance service is run by the Fire Services Department (FSD) Ambulance Command, moving three-quarters of a million patients a year, roughly 2,250 calls a day in 2024 alone. That volume, plus high-rise delays and dense urban logistics, rewards simple, reproducible decision support and crisp documentation for Hospital Authority EDs.
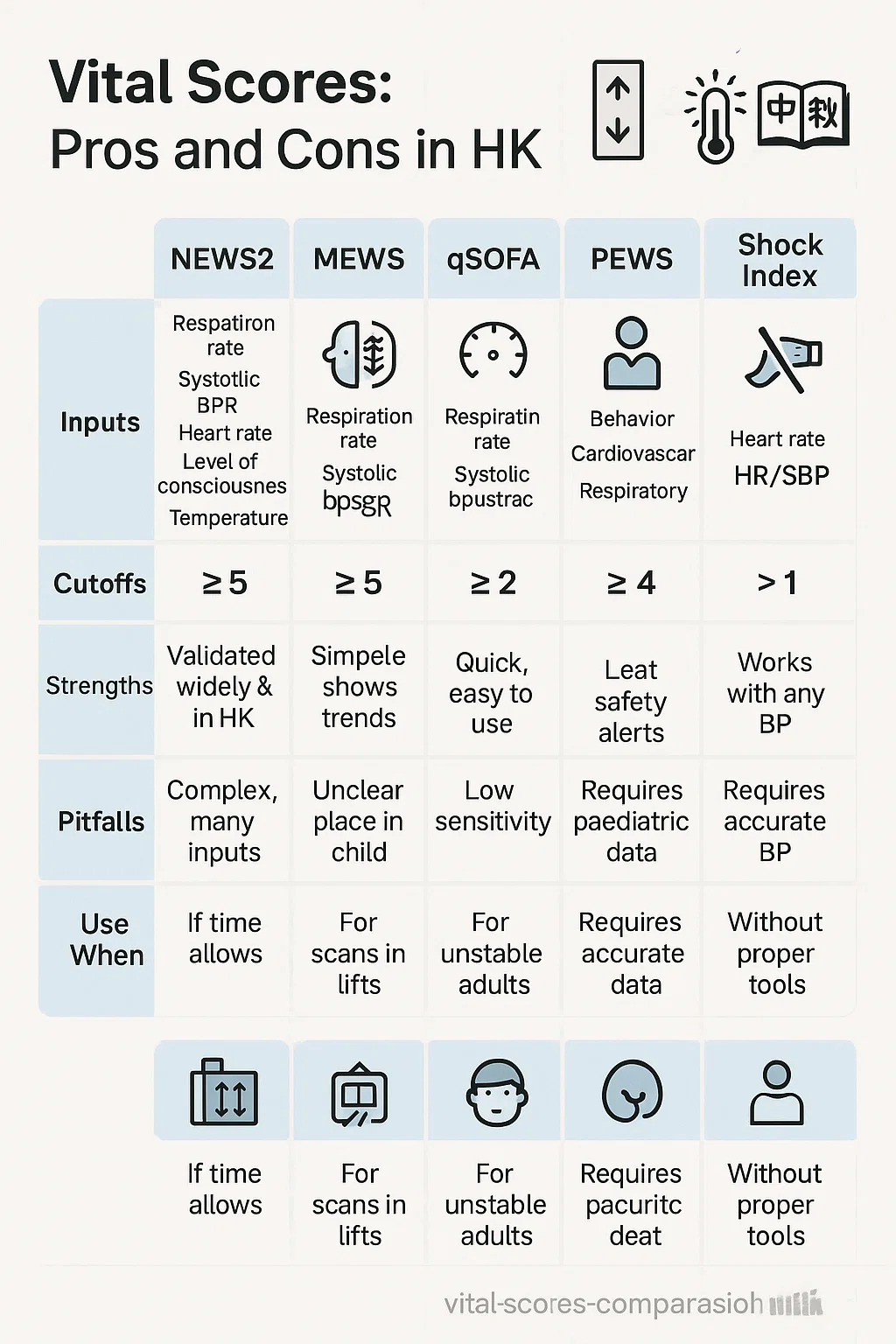
At the bedside, five tools routinely influence prehospital decisions worldwide: NEWS2, MEWS, qSOFA, pediatric PEWS variants, and the Shock Index (including trend ΔSI). Add waveform capnography to that bundle and you can read not just “how sick,” but “what system is failing and how fast.” Recent studies and guideline updates give us a clearer picture of each tool’s strengths and traps.
The core toolkit, compared
NEWS2: the generalist that travels well
NEWS2 aggregates six routine vitals with oxygen supplementation to flag deterioration and trigger escalation. Multiple recent studies both general and infection-focused show NEWS2’s strong discrimination for time-critical treatment compared with alternatives, making it a reliable default “sick/not sick” compass.
Where NEWS2 shines in Hong Kong
- Works off vitals you already collect at triage or doorstep.
- Sensitivity for deterioration beats quick sepsis screens like qSOFA in many cohorts, which matters when elevator delays and traffic stretch transport times.
- Easy to build into your tablet forms and bilingual handover notes.
Limits
- Not pediatric-validated; use PEWS flavors for kids.
- Oxygen weighting can over-trigger scores in chronic hypoxemia without a trend.
Pro Tip: NEWS2 ≥5 or any single parameter in red should auto-trigger “load and go” thinking unless you can rapidly correct the driver (e.g., hypoglycemia). Trend the score every lift stop: improving? hold the line; worsening? escalate early.
MEWS: the old workhorse
MEWS is simple, familiar, and still appears on many ward charts in Asia, including HA settings historically. It’s fine for quick gestalt reinforcement but trails NEWS2 in comparative performance.
Use it when: your receiving ED references MEWS in triage notes and you need a shared language.
Avoid over-relying when: sepsis or hypoxia is suspected; choose NEWS2 for better sensitivity.
qSOFA: still useful, but not your only sepsis screen
qSOFA (RR ≥22, SBP ≤100, altered mentation) is fast and spartan. Its appeal is speed; its weakness is missing early sepsis that isn’t hypotensive yet. Multiple analyses now favor NEWS2 over qSOFA for prehospital identification of high-risk infection.
Hong Kong take: If an elderly pneumonia patient in a Sham Shui Po walk-up is tachypneic with borderline saturation and normal SBP, qSOFA may shrug while NEWS2 pushes you to act. Use qSOFA as a “red flag,” not a sole gatekeeper.
Pediatric early warning (PEWS/ED-PEWS)
Children aren’t small adults. Pediatric early warning scores adjust for age-specific cutoffs and behavior cues. Recent multicenter work continues validating ED-focused PEWS variants for acute settings.
Hong Kong take: For febrile children in cramped flats, an age-adjusted tachycardia with prolonged cap refill and work-of-breathing changes should tip a PEWS rise and prompt early hospital prenotification.
Shock Index and ΔSI: the hidden bleeding detector
Shock Index (SI = HR/SBP) and its trend (ΔSI) catch occult hypoperfusion even when SBP looks “OK.” Prehospital data show SI ≥0.9 and upward trends associate with transfusion, urgent surgery, and mortality; a ΔSI >0.1 matters even in normotensive patients.
Why Hong Kong crews should care: In cramped stairwells, you may only get partial vitals. If HR is 120 and SBP 100 (SI 1.2) on the first landing, and SI climbs again at the lift lobby, you’re watching a decompensation in real time call the receiving ED, consider hemorrhage, and shorten scene time.
Capnography (EtCO₂): your ventilation and perfusion dashboard
Continuous waveform capnography confirms tube placement, tracks ventilation, and reflects perfusion during arrest and shock. The 2025 AHA Guidelines again emphasize capnography in resuscitation; 2024 research highlights trend-aware monitoring that correlates with outcomes.
At the curb:
- Intubated or supraglottic airway: maintain continuous waveform no waveform, no confidence.
- Spontaneously breathing shock or sepsis: nasal EtCO₂ guides ventilation coaching and hints at perfusion; a falling EtCO₂ with rising SI is a bad duet.
Quick comparison matrix
| Tool | Inputs | Typical Trigger | Best Use | Strengths | Watch-outs |
|---|---|---|---|---|---|
| NEWS2 | RR, SpO₂, O₂, Temp, SBP, HR, AVPU | ≥5 total or any red | General adult deterioration, infection | Strong sensitivity; easy trending | Not for pediatrics; O₂ weighting may over-trigger in chronic hypoxemia |
| MEWS | HR, SBP, RR, Temp, AVPU | ≥4–5 (local policy) | Legacy workflows | Familiar; simple | Lower discrimination than NEWS2 |
| qSOFA | RR, SBP, mentation | ≥2 | Rapid sepsis “red flag” | Fast bedside filter | Misses early sepsis; use with NEWS2 |
| PEWS / ED-PEWS | Age-adjusted vitals + behavior | Moderate/high risk bands | Febrile/respiratory kids | Pediatric-specific risk | Score choice varies; training needed |
| Shock Index / ΔSI | HR/SBP and change over time | SI ≥0.9 or Δ>0.1 | Trauma, hemorrhage, sepsis hypoperfusion | Flags occult shock; trend-friendly | Needs repeated measures; SBP accuracy matters |
| Capnography (EtCO₂) | Waveform + value | <10–12 mmHg in arrest; falls with low flow | Airway confirmation; ventilation titration; perfusion trend | Confirms ETT; tracks CPR quality; outcome correlation | Nasal adapters, dead space issues in neonates |
Field use in Hong Kong: scenarios and decisions
1) Elderly pneumonia in a 30-floor walk-up
Vitals: RR 28, SpO₂ 89% RA → 94% on 2 L, Temp 38.5, SBP 138, HR 104, A on AVPU.
- NEWS2: likely ≥5. Trend the score at each movement phase; if stable after oxygen and coaching, keep O₂ low to achieve target saturation and avoid hyperoxia.
- qSOFA: 0–1. Not helpful alone don’t downplay risk based on qSOFA.
- Capnography: Nasal EtCO₂ assists ventilation coaching; falling EtCO₂ with rising RR warns of impending fatigue.
Action: Early prenotification, consider sepsis pathway; minimize scene time.
2) Blunt abdominal trauma on a narrow street
First read: HR 110, SBP 118 (SI 0.93). Five minutes later: HR 124, SBP 104 (SI 1.19, ΔSI +0.26).
- ΔSI >0.1 predicts worse outcomes even if SBP hasn’t crashed; prioritize rapid transport, bleeding control, and ED alert for possible transfusion. Capnography: Declining EtCO₂ despite similar RR suggests falling perfusion; reassess volume status and external hemorrhage control.
3) Febrile child in a subdivided flat
Age-adjusted tachycardia, mild retractions, cap refill 3–4 s, SpO₂ 92% RA.
- PEWS/ED-PEWS flags moderate risk; combine with work-of-breathing assessment and hydration status.
- Action: Gentle oxygen titration, antipyretic per protocol, early prenotification if transport time is extended by lift or traffic delays.
Pro Tip: Use “two-step validation.” First, run the score (NEWS2, PEWS, etc.). Second, ask: Do the waveform and the trend agree? If EtCO₂ and ΔSI say “worse” while SBP looks okay, trust the trends and move. On-scene workflow that saves time (and face at handover)
The Hong Kong EMS vital-to-decision checklist
- Rapid baseline (≤60 s): RR, SpO₂, mental status, pulse quality, skin. Start the clock.
- First pass vitals: HR, SBP, Temp (if relevant), glucose. Record exact time and patient position (standing vs sitting).
- Run the right score:
- Adults: NEWS2; consider qSOFA only as an add-on red flag.
- Pediatrics: PEWS/ED-PEWS.
- Add perfusion lens: Calculate SI; plan to recalc in 3–5 minutes. Note mechanism and bleeding risk.
- Wire in capnography:
- Airway devices: continuous waveform or it didn’t happen.
- Spontaneous breathing and shock/sepsis: nasal EtCO₂ for trend.
- Treat drivers fast: oxygen to target, glucose correction, bleeding control, bronchodilator per SOP.
- Reassess & trend: NEWS2 trend, ΔSI, EtCO₂ direction.
- Call early with clarity: “Adult NEWS2 6, SI 1.1 rising by 0.2, EtCO₂ falling from 32 to 26 despite RR 26 suspected sepsis/low-flow.”
- Document bilingual essentials: numbers + trends + response to treatments; pain points (lift delays, confined space) that influence timelines.
- Handover like a headline: lead with the score and trend, then the story.
Documentation that sticks at triage
Hospital Authority ED triage runs a five-level system; crisp, standardized vital-to-trend summaries reduce re-triage friction for older adults and time-critical cases. Pack your handover with: the initial score, trend over the last 10 minutes, any ΔSI >0.1, EtCO₂ trajectory, and exact interventions. Template:
- “Male 78. SOB, fever. NEWS2 6→5 after 2 L O₂; SI 0.9 stable; EtCO₂ 32→34 with coached breathing. Likely pneumonia; prenotified.”
- “Female 44 post-MVC. SI 0.93→1.19 (Δ+0.26), EtCO₂ 30→24, abdominal tenderness; transport 12 min; bleeding control ongoing.”
What the latest evidence says (so you can defend your calls)
- NEWS2 vs qSOFA: In prehospital and ED cohorts, NEWS2 generally outperforms qSOFA for identifying high-risk infection and need for urgent treatment. Use qSOFA for “instant concern,” but default to NEWS2 for disposition.
- Early warning tools vary widely: 2024 comparative work across AI and classic scores shows large performance variability transparency and local validation matter. For street use, simpler and validated tools (NEWS2, PEWS) remain safe bets.
- Shock Index and ΔSI are not optional in trauma: Prehospital studies link SI ≥0.9 and ΔSI >0.1 with transfusion, urgent surgery, and mortality even before hypotension. That’s your cue to move.
- Capnography is standard and informative beyond tubes: 2025 AHA guidance and 2024 studies reinforce continuous waveform capnography for airway confirmation, CPR quality, and trend-based assessment that correlates with outcomes.
- System context: FSD Ambulance Command’s scale and operational tempo underline the need for structured, shareable metrics that travel well from lift lobby to ED bay.
Putting it together: a practical field algorithm
- First minute: Safety sweep, general impression, RR and mental status.
- Measure: HR, SBP, SpO₂, Temp (if indicated), BGL; start EtCO₂ if airway device or high suspicion of sepsis/shock.
- Score: Adult NEWS2, child PEWS. If infection suspected, note qSOFA but don’t let a “0–1” lull you.
- Perfusion check: Calculate SI; plan to repeat in 3–5 minutes.
- Treat cause: O₂ titration, bronchodilator, glucose, bleeding control, fluids per protocol.
- Reassess: NEWS2 trend, ΔSI, EtCO₂ direction. Any worsening trend = earlier move and prenotification.
- Communicate: Share the score and trend first, then the narrative.
- Document: Vital values, timing, body position, treatments, trends, delays (elevator, confined space), and language/communication needs.
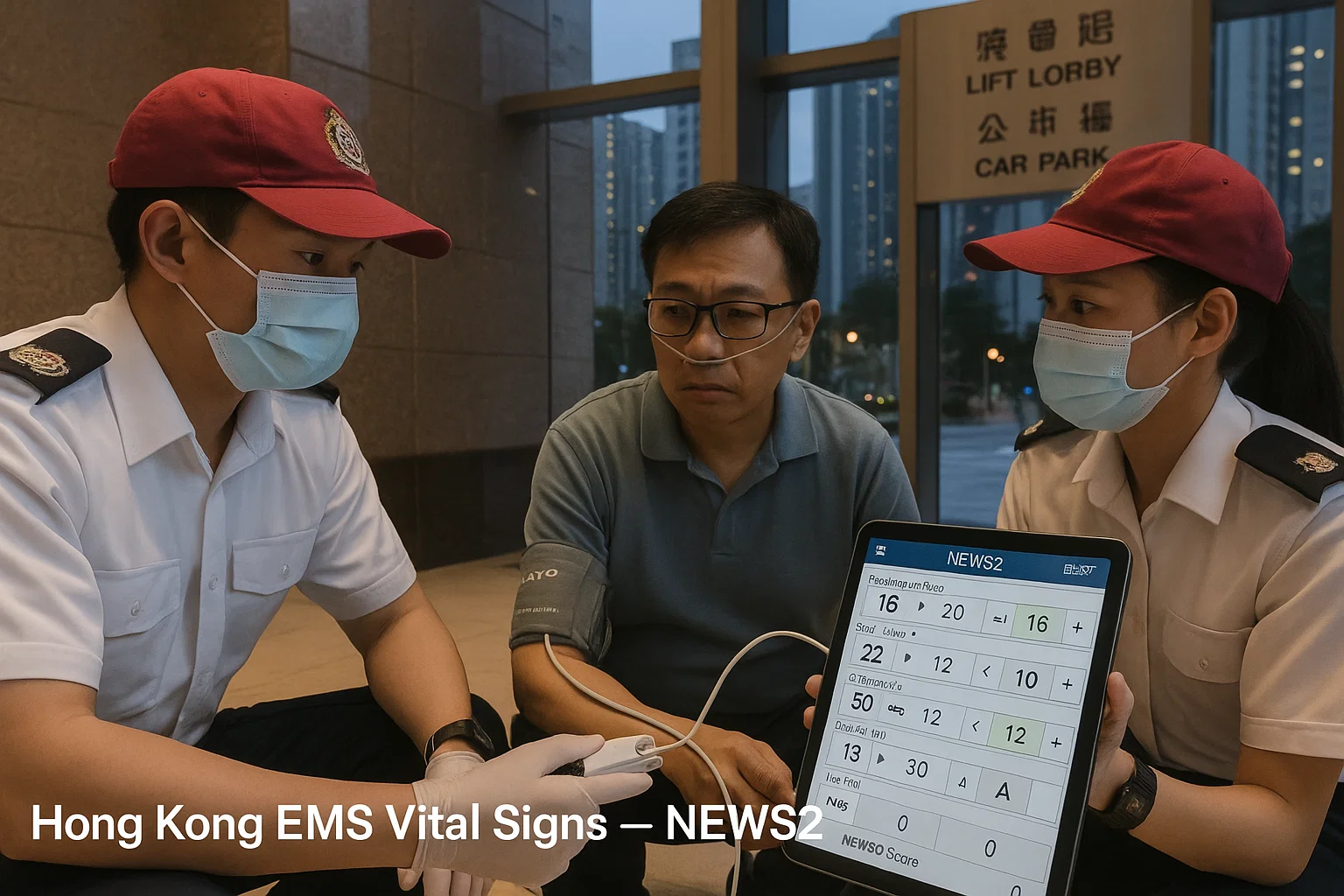
Image placement guide (for your training deck)
- Featured scene: FSD crew with tablet showing NEWS2, EtCO₂ nasal cannula in place, lobby signage in Chinese/English.
- Infographic matrix: NEWS2, MEWS, qSOFA, PEWS, SI/ΔSI inputs, triggers, “use when,” pitfalls.
- Scenario pair: Trauma ΔSI rise with falling EtCO₂ vs respiratory case with improving EtCO₂ after coaching and oxygen titration.
Common pitfalls (and how to avoid them)
- Treating a single SBP as truth. Arm position, cuff size, and motion artifacts lie. Always pair SBP with pulse quality, SI, and a repeat reading before you downgrade urgency.
- Ignoring oxygen side effects. High-flow O₂ can inflate NEWS2 via SpO₂/O₂ weighting and mask CO₂ retention. Titrate to target saturation and watch the EtCO₂ waveform.
- Using qSOFA as the gatekeeper. It’s fast but misses early sepsis; let NEWS2 lead disposition.
- No trend, no story. A single screenshot is weak evidence. Trend NEWS2, SI, and EtCO₂ especially during long carries or lift delays.
Mini-case documentation examples for Hong Kong
Case A Chronic lung disease exacerbation (Sham Shui Po):
- Initial: RR 30, SpO₂ 86% RA, HR 108, SBP 148, Temp 37.5, A on AVPU; EtCO₂ 32 with shallow waveform.
- After 5 min: SpO₂ 91% on 1–2 L, RR 26, EtCO₂ 36 with improved waveform.
- NEWS2 7→5, SI 0.73 stable, improved EtCO₂. Early notification done; careful O₂ titration documented. Case B Pedestrian struck (Mong Kok):
- Initial: HR 112, SBP 116 (SI 0.97), cool skin, narrow pulse pressure; EtCO₂ 28 on nasal sample.
- At 8 min: HR 126, SBP 100 (SI 1.26, Δ+0.29), EtCO₂ 24.
- Action: “Major trauma; ΔSI >0.1 with falling EtCO₂. Suspected intra-abdominal bleed. ETA 9.”
Training and QA suggestions for agencies
- Embed calculators for NEWS2, PEWS, SI/ΔSI on crew tablets with bilingual labels and auto-timestamping.
- Mock-call drills in high-rise settings to practice trending during movement.
- Capnography refreshers tied to 2025 AHA points: airway confirmation, CPR quality, ROSC prediction, ventilation guidance.
- Audit handovers for “score + trend first” phrasing and outcome correlation.
FAQ
Does Hong Kong ED triage use these scores directly?
HA hospitals use a five-level triage; early warning scores may inform in-hospital response but are most valuable prehospital as a common language for deterioration. Lead with the number and trend; triage will map it to their system.
Which single tool should I learn first?
NEWS2 for adults. It travels well, has good sensitivity, and integrates easily with your existing vitals set.
Is qSOFA obsolete?
Not obsolete just insufficient alone. Keep it for quick concern, but use NEWS2 to drive decisions.
How do I use Shock Index if SBP readings vary?
Repeat the measurement in the same position, check cuff fit, and focus on the trend (ΔSI). A rise >0.1 is meaningful even if SBP never dips below 90.
What’s new with capnography?
The 2025 AHA guidelines reiterate continuous waveform capnography for airway confirmation and quality of resuscitation; 2024 studies emphasize the value of tracking EtCO₂ trends, not just one value.
Copy-ready How-To (procedural) steps
How to convert raw vitals into a reliable handover (Hong Kong EMS)
- Capture RR, mental status, SpO₂; start timer.
- Record HR/SBP, Temp if indicated; note posture.
- Run adult NEWS2 or PEWS for kids; optionally note qSOFA for infection.
- Compute SI, plan to repeat in 3–5 minutes.
- Start capnography (waveform) if airway device or suspected sepsis/shock.
- Titrate O₂, correct glucose, control bleeding, bronchodilate as indicated.
- Reassess and trend: NEWS2, ΔSI, EtCO₂.
- Communicate trend first, then narrative; prenotify early if any worsening trend.
- Document bilingual numbers, trends, interventions, and environmental delays.
- Handover headline: “Score + trend” → “primary problem” → “treatments.”
Closing take
Bottom line: in Hong Kong’s high-volume, high-rise reality, NEWS2 + SI/ΔSI + waveform capnography gives you the fastest, most defensible path from numbers to decisions. Use PEWS variants for children, keep qSOFA as a quick flag not a barrier and hand over with trends, not just snapshots. That’s how you shave minutes, avoid misses, and earn trust at the triage desk.

Alex Smith, a seasoned medical technician with 15 years in ambulance services, writes crucial first-aid tips and emergency care insights on arescuer.com.
