
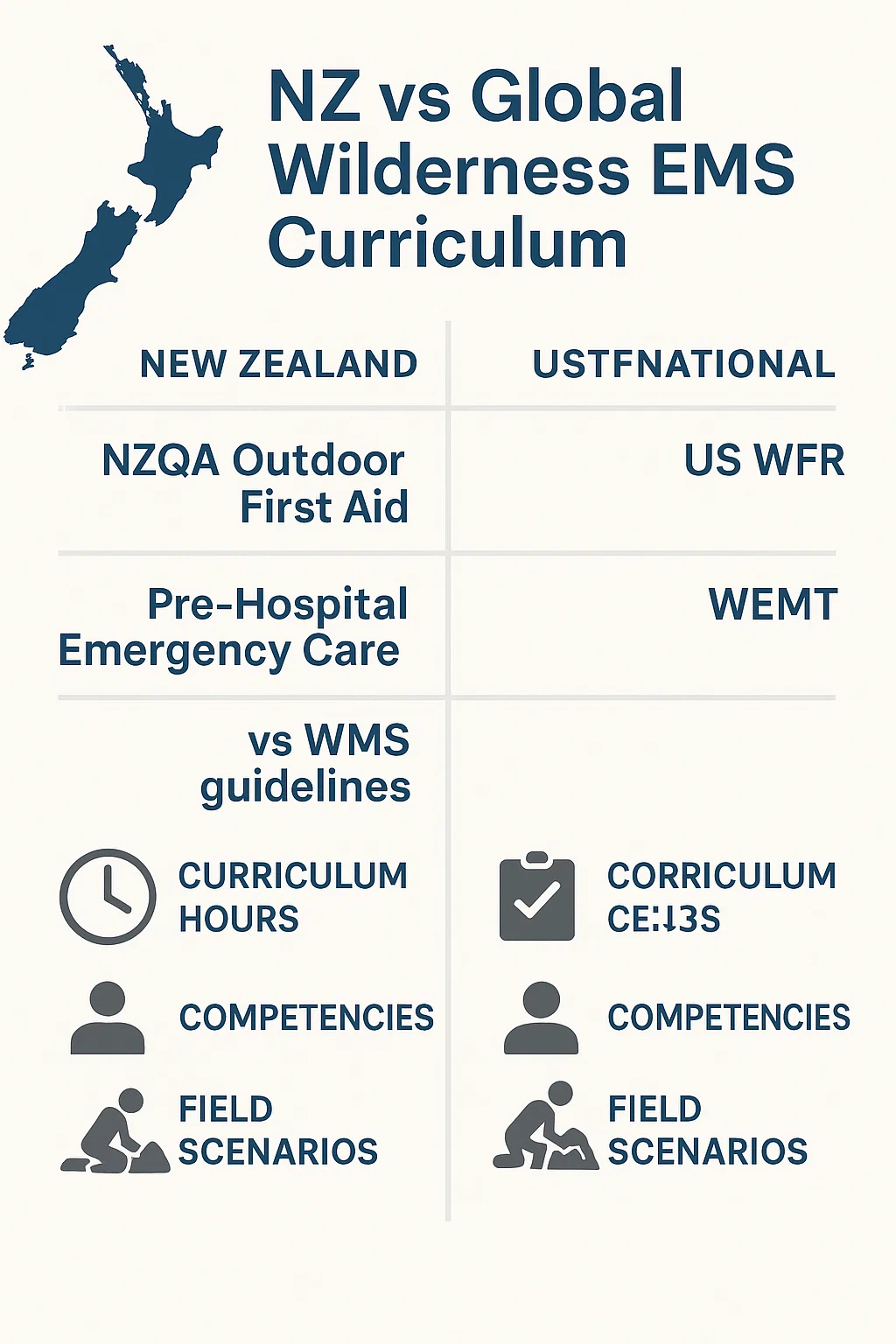
Here’s what matters: New Zealand has solid foundations in outdoor first aid and pre-hospital care, but the global field has pushed ahead with clearer tiered models, longer training hours, and tighter linkages between wilderness protocols and mainstream EMS. This comparison walks through where New Zealand stands, where it excels, and where aligning with international standards could raise the bar.
Why Wilderness Medicine Matters in Aotearoa
Remote medicine isn’t a niche in New Zealand. It’s everywhere alpine routes, tramping tracks, rivers, isolated farms, adventure tourism, offshore boating, and multi-day SAR operations. Even small gaps in training show up quickly in the field.
Three realities drive the need for strong curriculum here:
- Distance and delay
Rescue time can stretch from minutes to hours. Decision-making becomes far more than ABCs. - Weather and terrain extremity
Hypothermia, falls, river entrapment, and environmental injuries are routine risks. - Limited evacuation options
Helicopter availability, daylight windows, and wind become clinical variables.
International systems like NOLS WFR, WEMT, and Wilderness Medical Society guidelines build entire sections around these variables. NZ’s current training touches them but often not with the same depth or structure.
How Global Wilderness Medicine Curricula Are Structured
Before comparing New Zealand, it helps to outline the international “gold standard” framework. Across the US, Canada, Europe, and parts of Asia, several consistent features appear.
1. Tiered Pathways
Most countries separate wilderness training into recognisable levels:
- Wilderness First Aid (WFA) – 16–20 hours
- Wilderness First Responder (WFR) – 70–80 hours
- Wilderness EMT / WEMT – 180+ hours
- Advanced Wilderness Life Support – specialised modules
- Continuing practice requirements – skill refresh every 2–3 years
These levels allow easy recognition, upgrading, and interoperability.
2. Strong Scenario-based Learning
Global providers run dozens of scenarios: night rescues, improvised splinting, long-term patient care, multi-casualty events, and simulated evacuations.
3. WMS Practice Guidelines Integration
From anaphylaxis to frostbite to lightning injury, wilderness medicine in the US/Canada is anchored to the Wilderness Medical Society updates (2024–2025 editions).
These are evidence-based and updated annually.
4. Unified EMS Conversion
A WEMT can often crosswalk into urban EMT with additional modules, creating a fluid professional pathway.
This clear structure is the main difference when you place NZ alongside it.
New Zealand’s Current Wilderness/Remote EMS Framework
New Zealand uses NZQA unit standards, outdoor training providers, SAR agency courses, and ambulance service education pathways. The quality varies from strong to inconsistent depending on the provider and level.
Core NZ Elements
- NZQA Outdoor First Aid (Level 2–3)
Good for basic outdoor workers, but typically 8–12 hours. Not enough for serious wilderness decision-making. - Pre-Hospital Emergency Care (PHEC)
Excellent for responders, event medics, and SAR volunteers. Strong hands-on focus but not designed specifically for long-term wilderness care. - Ambulance service education (EMT/Paramedic)
Professionally solid, but urban-centric in many areas. Wilderness modules exist, but vary by region. - SAR-specific medical refreshers
Good scenario work, but not part of a standardised national ladder.
What’s Missing Compared to Global Benchmarks
Here’s the simple truth: NZ has capability but lacks a nationally unified wilderness medicine curriculum. Different providers teach to different hours, different scenarios, and different interpretations of remote care.
The gaps usually appear in:
- Contact-hour depth
Many NZ courses are 8–24 hours. Global equivalents run 40–80+ hours. - Long-term patient care
NZ training often assumes rescue within hours; global wilderness training assumes delays up to a day or more. - Wilderness-specific medical protocols
WMS-guideline integration is patchy. - Credential naming consistency
“Outdoor First Aid” and “PHEC” don’t map easily to WFA/WFR/WEMT naming. - Upgrade pathways
International responders know exactly how to move from WFA → WFR → WEMT.
NZ responders must jump between unrelated certification structures.
New Zealand vs Global Benchmarks
Training Hours
| Training Type | New Zealand Typical Hours | Global Standard |
|---|---|---|
| Basic Outdoor First Aid | 8–12 hrs | 16–20 hrs (WFA) |
| Intermediate Remote Care | 12–24 hrs | 40–60 hrs (bridging) |
| High-level Wilderness | PHEC 20–40 hrs | 70–80 hrs (WFR) |
| Remote EMT Level | None Standardised | 180+ hrs (WEMT) |
New Zealand’s strength is efficiency; its weakness is depth.
Scenario-Based Training
New Zealand strengths
- Strong SAR training culture
- Well-adapted to local terrain
- Realistic rope, alpine, and bush scenarios
Global strengths
- Structured, tiered scenario complexity
- Multiple-night practicals
- Emphasis on long-term field care and evacuation planning
Both systems value realism, but global programmes formalise it better.
Medical Guidelines Integration
Global providers base nearly every teaching point on:
- WMS Practice Guidelines (2024–2025)
- NAEMT wilderness extensions
- Prehospital Trauma Life Support wilderness modifications
In NZ, integration varies by instructor and organisation. It’s not a national requirement.
Evacuation & Field Management Skills
New Zealand excels in terrain-specific skills:
- river crossings
- alpine movement
- boat-based retrieval
- helicopter safety
- improvised carry systems used in SAR
Where NZ can strengthen is in:
- delayed evacuation medical planning
- field treatment algorithms for 6–24 hour care
- wilderness pharmacology variations
- prolonged field care (PFC) principles
Modern remote EMS expects these components.
Where New Zealand Performs Exceptionally Well
It’s not a one-sided comparison. NZ has clear advantages:
1. Local Terrain Expertise
Training here reflects the realities of the Southern Alps, Fiordland, bush, and marine environments. No imported curriculum can beat that.
2. Strong SAR Culture
LandSAR, Coastguard, and alpine rescue groups maintain practical skills at a high standard.
3. Adaptive Problem-Solving
New Zealand responders are trained with a “make do with what you have” mindset. That’s gold in wilderness medicine.
4. Integration with Outdoor Industry
Guides, instructors, adventure tourism operators, and DOC staff feed back field experience that influences training.
The foundation is strong what NZ needs is unified structure around it.
Key Weaknesses That Limit Interoperability
1. International Recognition
A PHEC certificate does not translate well overseas.
WFR and WEMT are widely recognised globally; NZ equivalents are not.
2. Inconsistent Curriculum Hours
Great instructors exist in NZ, but their course lengths differ widely.
3. No National Wilderness Certification Ladder
Responders can’t simply move from Level A → B → C the way they can overseas.
4. Limited Prolonged Field Care (PFC) Exposure
PFC is now standard in many global remote EMS curricula due to climate disasters, long delays, and remote trekking.
New Zealand training rarely covers:
- long-term airway monitoring
- delayed fluid management
- extended hypothermia management
- extended wound care
- 12–24 hour patient monitoring
The need is growing.
What a Modern Wilderness Curriculum Should Include for New Zealand
Here’s what a well-structured, NZ-aligned curriculum would look like if built to global benchmarks but tailored to our landscape:
Tier 1 – Wilderness First Aid
- Basic patient assessment
- Common environmental injuries
- Scene management in bush & alpine settings
- Short delays in evacuation
Tier 2 – Wilderness First Responder
- Trauma care in delayed evacuation
- Musculoskeletal injury management
- Spine injury protocol decisions
- Environmental extremes (NZ-specific winds, cold, water hazards)
- Night rescue operations
- Multi-casualty bush scenarios
- Leadership and comms in remote settings
Tier 3 – Wilderness EMT
- Advanced airway management
- Pharmacological modifications in remote settings
- Hydration & field IV/IO considerations
- Extended care for 12–24 hours
- Evacuation planning
- Coordination with helicopter/EMS units
Annual Refresh Structure
- Skills recert annually
- Scenario refresh every 24 months
- WMS guideline updates integrated automatically
This kind of structure brings NZ responders up to global operability without losing local character.
Should New Zealand Fully Adopt Global Models?
Not entirely. New Zealand’s environment demands local nuance. But aligning with international tiers WFA, WFR, WEMT would improve recognition, consistency, and professional mobility.
The right solution is hybrid:
- Keep NZ’s terrain knowledge and SAR strengths
- Combine with global medical structure and depth
This blend would produce world-class wilderness responders.
What Agencies Should Update First
For training providers
- Increase minimum hours for wilderness courses
- Integrate WMS guidelines formally
- Add long-term patient scenarios
- Build a clear certification ladder
For SAR teams
- Refresh prolonged field care modules
- Anchor protocols to international wilderness EMS standards
- Standardise cross-team medical expectations
For outdoor industry employers
- Move staff training from “basic outdoor first aid” to “WFR-equivalent” levels
- Require recertification cycles rather than lifetime certificates
For ambulance and EMS services
- Develop wilderness bridges into EMT/Paramedic pathways
- Include remote decision-making modules for juniors
Closing Thoughts
Bottom line: New Zealand has the right people, the right field experience, and some of the best SAR capability anywhere. What’s missing is a cohesive structure that matches what top international programmes have refined over decades.
Once NZ aligns its wilderness medicine and remote EMS curriculum with global benchmarks while keeping its terrain-specific strengths it will produce some of the most capable remote medical responders in the world.

Emma Lee, an expert in fire safety with years of firefighting and Rescuer experience, writes to educate on arescuer.com, sharing life-saving tips and insights.
