Upon completion of this lesson, you will be able to:
- Define an open fracture and closed fracture, and list four signs and symptoms.
- Define a dislocation, a sprain, and a strain and list four signs and symptoms.
- Give two reasons for immobilizing a fracture, a sprain or a strain on a patient.
Demonstrate the Pre-hospital treatment of fractures and dislocations of the extremities, hips, and shoulders.
Skeletal System
The adult skeleton is composed of 206 bones. The human skeleton consists of two main divisions, the axial skeleton, and the appendicular skeleton. 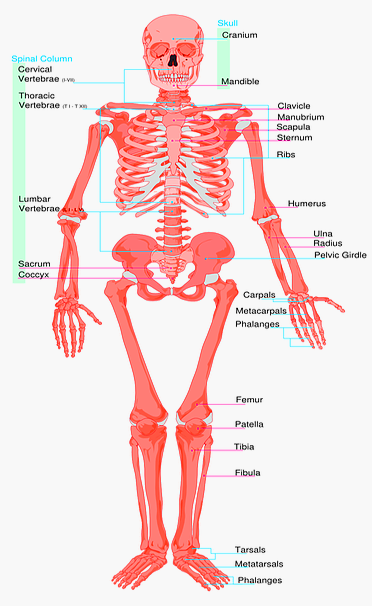
Functions of the skeletal system
- Provides a Shap for the body
- Protects vital Organs
- Provides safety for the Human body
- Produces cells
Axial Skeleton
The axial skeleton (at right) consists of 80 bones, including:
- Skull
- Thorax
- Vertebral (spinal) column
Appendicular Skeleton
The appendicular skeleton (below, right) consists of 126 bones which include:
- Shoulder: clavicle and scapula
- Upper extremities: arms, hands, fingers
- Pelvis (hips)
- Lower extremities: legs, feet, toes
Joints (articulations)
Joints are bone ends that fit into each other. There are several types of joints:
- Immovable joints, such as in the skull
- Slightly movable joints, such as the spine
- Freely movable joints, such as the elbow or knee joints (hinge) or the hip joint (ball and socket)
Ligaments and Tendons
• Ligaments connect and hold bones together at the joints
• Tendons attach the skeletal muscles to the bone. These muscles control the movement of the joints.
Fractures, Dislocations, and Sprains
Fractures
Definition: Any break in the continuity of a bone.
Fractures can be open or closed.
Closed injury: One in which the overlying skin is intact. Proper splinting helps prevent the closed fracture from becoming an open fracture.
Open injury: One in which the skin has been broken or torn either from the inside by the injured bone or from the outside by the object that caused the penetrating wound with the associated bone injury. The bone may or may not protrude through the wound.
Open fractures are serious because of the risk of contamination or infection is greater. You can see Infectious Diseases Signs and Symptoms.
Treat life-threatening injuries first. It is impossible to rule out a fracture through a physical exam of the patient. Many sprains and dislocations present signs and symptoms similar to a fracture.
Dislocation
Dislocation: Injury in which a bone is moved out of its normal position in a joint and remains that way.
A dislocation sometimes causes the tearing of ligaments and soft tissues if stretched far beyond the normal range of motion. The shoulder, elbow, fingers, hips, and ankles are the joints most frequently affected. Signs and symptoms of dislocation are similar to those of a fracture.
Sprains and Strains
Sprain: Injury in which ligaments are stretched or partially torn, commonly associated with joint injuries
Note: Do not confuse a sprain with a strain, which involves muscle injury.
Strain: Injury in which a muscle or a muscle and tendon are over-extended.
Dislocation, fracture and sprain may all be present in an injury.
Signs and Symptoms of a Musculoskeletal Injury
- Deformity or angulation: compare with the opposite limb
- Pain and tenderness upon palpation or movement
- Crepitus (grating) – a sound or feeling of broken bone ends rubbing together
- Swelling
- Bruising or discoloration
- Exposed bone ends
- Joint locked in position – reduced motor ability or reduced ability to articulate a joint
- Numbness and paralysis – may occur distal to the site of injury caused by bone pressing on a nerve
- Circulatory compromise distal to injury evidenced by alteration in skin colour, temperature, Dulse or capillary refill
Note: NEVER intentionally induce crepitus. This may cause or aggravate soft tissue injury.
Splinting
Definition: Applying a device to stabilize any painful, swollen, or deformed body part.
The primary objective of splinting is to prevent further movement of body parts. For any splint to be effective, it must immobilize adjacent joints and bone ends.
Reasons for splinting include:
- Immobilize a limb
- Decrease swelling
- Sprains
- lacerations
- Fractures
- Dislocations
- Painful joints
- Inflammatory disorders
Types of Splints
Effective splinting may require some ingenuity. Though you may carry many types of splinting devices, many situations will require you to improvise.
Five basic types of splints
- Rigid splint: Requires limb to be in anatomical position. Ideal for long-bone injuries.
- Conforming splint: Can be molded to different angles to surround the extremity
- Traction splint: Used specifically for femur fractures.
- Sling and swathe: Two triangular bandages used to hold an injured arm in place against the body.
- Improvised splints: A book, cardboard, pillow or blanket, etc.
General Rules for Splinting
Regardless of the method of splinting, general rules apply to all types of immobilization, as follows:
- Always communicate your plans with your patient, if possible.
- Before immobilizing an injured extremity, expose and control bleeding.
- Always cut away clothing around the injury site before immobilizing the joint. Remove all jewelry from the site and below it.
Assess pulse, motor function and sensation (P.M.S.) - If the limb is severely deformed or distal circulation is compromised (cyanosis distal to fracture site or no distal pulse), align the bone with gentle traction (pulling). If pain or crepitus worsens, discontinue. Always follow local protocol.
- Do not attempt to push protruding bone ends back into place. However, when realigning, they may slip back into place. Make a note if this occurs.
- For patient comfort and proper immobilization, pad voids between the body and the splint, since many rigid splints do not conform to body curves.
- Pad the splint before applying it.
- If a joint is injured, immobilize it and the bones above and below. AVOID TUNNEL VISION.
- Do not over-splint the patient. In multi-system trauma patients, do not be distracted from life-threatening injuries by the gross appearance of non-critical injuries.
- Securing the patient to a long spine board supports and splints every bone and joint in one step without wasting time.
Pre-hospital Treatment for Suspected Fracture,
Dislocation or Sprain
Examining involves the use of your senses and skills of inspection (looking), palpation (feeling) and auscultation (listening). Use universal precautions and secure the scene.
1. Perform initial assessment
- Identify and treat major problems.
- Do not be distracted by the fracture.
- Remember cervical collar and oxygen, if applicable.
2. Perform a physical exam.
You can use the mnemonic “D.O.T.S.” to guide your exam as you look for signs and symptoms of injuries.
- Check for visible. Check all joints and bones through the entire length of the body.
- Check for, common with extremity
injuries. - Palpate for fracture, which may underlie injury without
deformity. - Check for stabilizing.
For extremity injuries, always assess for a distal pulse, motor function and sensation of(P.M.S.), before and after splinting.
Pulse: Radial in upper extremity injuries, dorsalis pedis (top of the foot) or posterior tibial pulse (back of ankles, medially) for lower extremities.
Motor function: Check the patient’s ability to move, such as wiggling toes or fingers (movement indicates intact nerves).
Sensation: Gently squeeze or pinch one extremity then the other, asking if the patient can feel your touch.
3. Stabilize the injury.
After completing a physical exam, secure the injury site providing manual stabilization. Do not release manual stabilization of an injured extremity until it is properly and completely immobilized.
4. Expose the injury. Cutaway clothing and remove jewelry before swelling occurs.
5. Treat open wounds and control bleeding. Cover with a clean or sterile dressing, avoid direct pressure over broken bone ends. Use pressure points as needed if bone ends protrude from injury, use caution not to allow bone ends to re-enter wound.
6. Prepare your splinting materials.
7. Carefully splint individual fractures. Caution: Be careful not to restrict circulation.
8. Treat for shock.
Pre-hospital Treatment for Specific Injuries and Application of Splints
Splinting the Upper Extremities
IMPORTANT: Always check pulse, motor function and sensation before and after splinting.
Shoulder and Clavicle
Signs and symptoms: Shoulder appears to be “dropped,” deformity (asymmetry), pain.
Treatment: Apply a sling and swath. Provide any padding necessary to fill the void between body and arm.
Humorous (shoulder)
Signs and symptoms: Pain, swelling, deformity
Treatment: Apply a rigid splint to the outside of the arm, pad voids, then apply sling and swath
Elbow
Important: Splint in the position found – do not attempt to straighten.
Signs and symptoms: Pain, swelling, deformity
Treatment: If the arm is bent at the elbow, splint with sling and swath alternate is pillow or blanket. If the elbow is straight, splint the entire arm, armpit to fingertips, both sides.
Forearm and Wrist
Signs and symptoms: Pain, swelling, deformity
Treatment: Splint area with arm board, then sling and swath. (Pneumatic splints are an option.)
Hands and Fingers
Important: Pulse can be checked by a capillary refill.
Signs and symptoms: Pain, swelling, deformity
Treatment: If one finger is fractured, tape it to an adjacent finger or use a tongue depressor to the splint. If more than one finger is fractured, splint the entire hand in the position of function. Place a roll of bandage in the palm of the hand, or other objects, then wrap entire hand and place on arm board.
Also, read about Medical Basic Training Course
Splinting the Lower Extremities
Pelvic Injuries
- Pelvic injuries can be life-threatening due to.
- Suspect shock.
- Any force strong enough to injure the pelvis can also injure the
Signs and symptoms
- Pain, especially when pressure is applied to iliac crests or pelvic bones
- Inability to lift legs while lying on the back
Pre-hospital treatment for a pelvic injury
- Minimize patient movement.
- Do not log roll or lift with pelvis unsupported.
- Place a folded blanket between the patient’s legs from groin to feet and bind together with cravats (2 upper leg, 2 lower leg).
- Place the patient on a long backboard.
- Treat for shock.
Hip Injuries
With this type of injury, it is difficult to differentiate an upper femur fracture from a hip or pelvic fracture or dislocation. Assess for life-threatening injuries as with pelvic injuries.
Signs and symptoms of the hip injury
- Pain
- Swelling
- Discoloration
- Inability to move leg(s)
- Possible foot rotation (outward or inward)
Pre-hospital treatment for hip injuries
- Bind legs together with a folded blanket between patient’s legs.
- Support the hip with pillows
- Stabilize patient on long backboard, or use longboards along the outer thigh, from foot to armpit with padding and along the inner thigh, from groin to foot.
- Secure with cravats.
Femoral Injuries
A femoral fracture can produce massive internal bleeding. Treat life-threatening conditions first.
Signs and symptoms of femoral fracture
- Pain (often intense)
- Deformity
- Rigidity
- Shortened limb
Pre-Hospital Treatment
If you find the leg in a straight position, use two padded boards — one along the inner thigh from groin to the foot and the other along the outer thigh from the armpit to the foot. Secure with cravats.
Knee Injuries
Signs and symptoms:
- Pain
- swelling
- deformity
Bent position: Immobilise in the position found. The bones above and below it should be splinted with short padded boards.
Straight position: Use two padded longboards, the first on the inner thigh from groin to beyond foot. Place the second on the outer thigh, from hip to beyond foot. Secure with cravats.
Tibia or Fibula Injury
Signs and symptoms:
- Pain
- swelling
- deformity
Pre-Hospital Treatment:
Pneumatic splint, two padded longboards – groin to foot and thigh to foot. Secure with cravats. Alternative method for a closed injury to the tibia or fibula is to use a circumferential splint.
Read about CPR & FBAO
Ankle and Foot Injuries
Signs and symptoms:
- Pain
- swelling
- deformity
Pre-Hospital Treatment: Stabilize, remove shoes and socks if possible (expose injury). A circumferential or formable splint such as a pillow secured with cravats is recommended.
Alternative: Two padded boards (splints) placed diagonally from mid-lower leg to ankle and secure with cravats

Alex Smith, a seasoned medical technician with 15 years in ambulance services, writes crucial first-aid tips and emergency care insights on arescuer.com.
