
Across NHS England, more than 25 million emergency handovers occur yearly. Each one is a potential weak link unless the right information travels fast, clear, and complete. That’s why structured pre-arrival communications, through radio or telephone, remain the backbone of safe adult patient transfers.
Why Pre-Arrival Notifications Matter
The Joint Royal Colleges Ambulance Liaison Committee (JRCALC 2024) defines pre-alert as “advance communication of a patient’s clinical status to prepare receiving facilities for immediate care.” NHS England echoes this in its Handover Improvement Framework (2024 edition) a concise, consistent pre-alert cuts handover delays by up to 43 seconds per patient, or roughly 12 hours saved daily in a medium-size ED.
Key outcomes of effective pre-alerts include:
- Optimized team readiness: resuscitation bay prepared, consultants notified.
- Improved triage: patient directed to correct clinical area on arrival.
- Reduced duplication: eliminates repeated assessment and confusion.
- Data integration: modern EPR systems capture radio data for traceability.
Yet surveys from the College of Paramedics 2024 Handover Audit show that one in six crews still face “handover friction” due to missing or poorly sequenced information. The fix lies in disciplined communication.
Core Communication Channels
UK EMS crews use two main modes:
- Radio (Airwave / ServiceNet) primary for real-time contact with ED or control rooms.
- Telephone (Landline / Mobile) secondary or backup channel when radio coverage is poor or for confidential updates (e.g., mental-health crises).
Digital supplements now add NHS EPR integrations platforms such as Cresta, Cleric EPCR, and C3 Cloud which auto-transmit pre-alert templates directly into the hospital’s digital whiteboard.
The Standard Framework: ATMIST & SBAR
The UK’s structured language for pre-alerts is ATMIST, occasionally coupled with SBAR for inter-service coordination.
| ATMIST Element | Meaning | Example (Adult Trauma) |
|---|---|---|
| A | Age | “Male, 46 years” |
| T | Time of incident | “Occurred 25 minutes ago” |
| M | Mechanism of injury | “High-speed RTC, frontal impact 40 mph” |
| I | Injuries found / suspected | “Deformity to right femur, chest bruising” |
| S | Signs (vitals) | “BP 90/60, HR 120, SpO₂ 94% on O₂” |
| T | Treatment given | “IV fluids started, morphine 5 mg, splint applied” |
For medical emergencies, switch “Mechanism” to “Main medical complaint” and adjust accordingly.
SBAR Situation, Background, Assessment, Recommendation is often used between clinicians once the patient reaches hospital, yet many ambulance trusts (e.g., NWAS and LAS 2024) encourage SBAR phrasing during telephone updates to duty consultants.

The Pre-Alert Call: Timing and Content
The golden rule: call as soon as critical information is stable but early enough for the ED to act.
- Trauma / Stroke / STEMI: usually 5–10 minutes pre-arrival.
- Sepsis or medical collapse: once diagnosis suspected and vitals recorded.
- Major incidents: immediately upon scene confirmation via control room.
A model script:
“This is Paramedic Alex from South East Ambulance, ETA 8 minutes.
Male 46, RTC frontal impact. Suspected femur fracture, BP 90/60, HR 120.
IV fluids running, morphine administered, cervical collar applied.
Requesting resus bay 1 and orthopaedic review on arrival.”
Concise, clear, and chronological the ATMIST backbone in human language.
Telephone vs Radio: When and Why
Radio is preferred for speed and multi-listener broadcast. It allows control room logging and automatic time-stamp.
Telephone excels for privacy and complex updates (e.g., safeguarding, end-of-life transfers). NHS Guidance (Gateway ref 2024-ENG-444) advises a secondary phone follow-up when:
- Information exceeds 60 seconds of radio time.
- The receiving clinician requests lab data or EPR identifiers.
- Radio congestion occurs during regional major incidents.
Integrating NHS Digital Tools
The UK is moving beyond voice-only pre-alerts. Modern systems such as:
- Cresta EPR Notifier: auto-populates ED boards from the crew’s ePCR device.
- Cleric EPCR Link: sends pre-alert data (BP, SpO₂, mechanism) via encrypted 4G.
- C3 Cloud: connects ambulance units to NHS Spine, ensuring that pre-arrival alerts become part of the national record.
According to NHS Digital Pilot Report 2025, hospitals using integrated pre-alerts cut “door-to-treatment” time for trauma patients by 9 minutes average.
Pro Tip Digital First:
Always verify the confirmation receipt on your tablet screen before assuming the hospital received the data. Loss of signal ≠ successful handover.
Common Pitfalls and How to Avoid Them
| Pitfall | Impact | Prevention Strategy |
|---|---|---|
| Missing mechanism or vitals | Mis-triage on arrival | Stick strictly to ATMIST order |
| Overloaded speech | Receiver misses key data | Pause every 3 phrases; confirm acknowledgment |
| Late pre-alert | No team ready | Trigger call ≥ 5 min before arrival |
| Unclear hospital destination | Routing confusion | Confirm with control room first |
| Dual radio channels | Cross-talk errors | Identify trust channel each transmission |
The Human Side of Structured Communication
Every communication protocol depends on human rhythm. Stress, fatigue, and environmental noise interfere with clarity. UK ambulance services combat this through:
- Simulation drills (per College of Paramedics training 2024).
- Crew role assignment (“caller” vs “driver”).
- Headset discipline radio mic two inches from mouth, no background chatter.
A study by NHS Improvement (2024) found that paramedics trained with structured speech and confirmation loops (“read-back received”) reduced handover errors by 28 percent.
Pro Tip Keep It Human:
Even with structured acronyms, empathy matters. Tone tells the ED how urgent you feel it is clarity plus calm equals confidence.
Practical Checklist Before Making the Pre-Alert Call
- ✅ Confirm hospital destination and capacity status.
- ✅ Stabilize critical airway and breathing issues.
- ✅ Collect vitals (BP, HR, RR, SpO₂, GCS).
- ✅ Identify mechanism or main medical complaint.
- ✅ Note treatments given and patient response.
- ✅ Prepare concise ATMIST summary on ePCR.
- ✅ Ensure radio channel or phone number ready.
- ✅ Gain crew consensus on who will speak.
- ✅ Transmit clearly and await acknowledgment.
- ✅ Document time of pre-alert in ePCR log.
This 10-step pre-alert checklist mirrors the NHS Handover 10-Point Safety List (2024) for national consistency.
When to Send a Secondary Update
Situations evolve. JRCALC 2024 recommends follow-up notification if:
- Vitals change > 20 percent.
- Additional interventions (e.g., intubation or blood products) occur.
- ETA changes by ≥ 5 minutes.
- Hospital diverts due to capacity.
Digital EPCR systems can auto-prompt crews for an update if ETA variance exceeds threshold an advantage radio cannot offer.
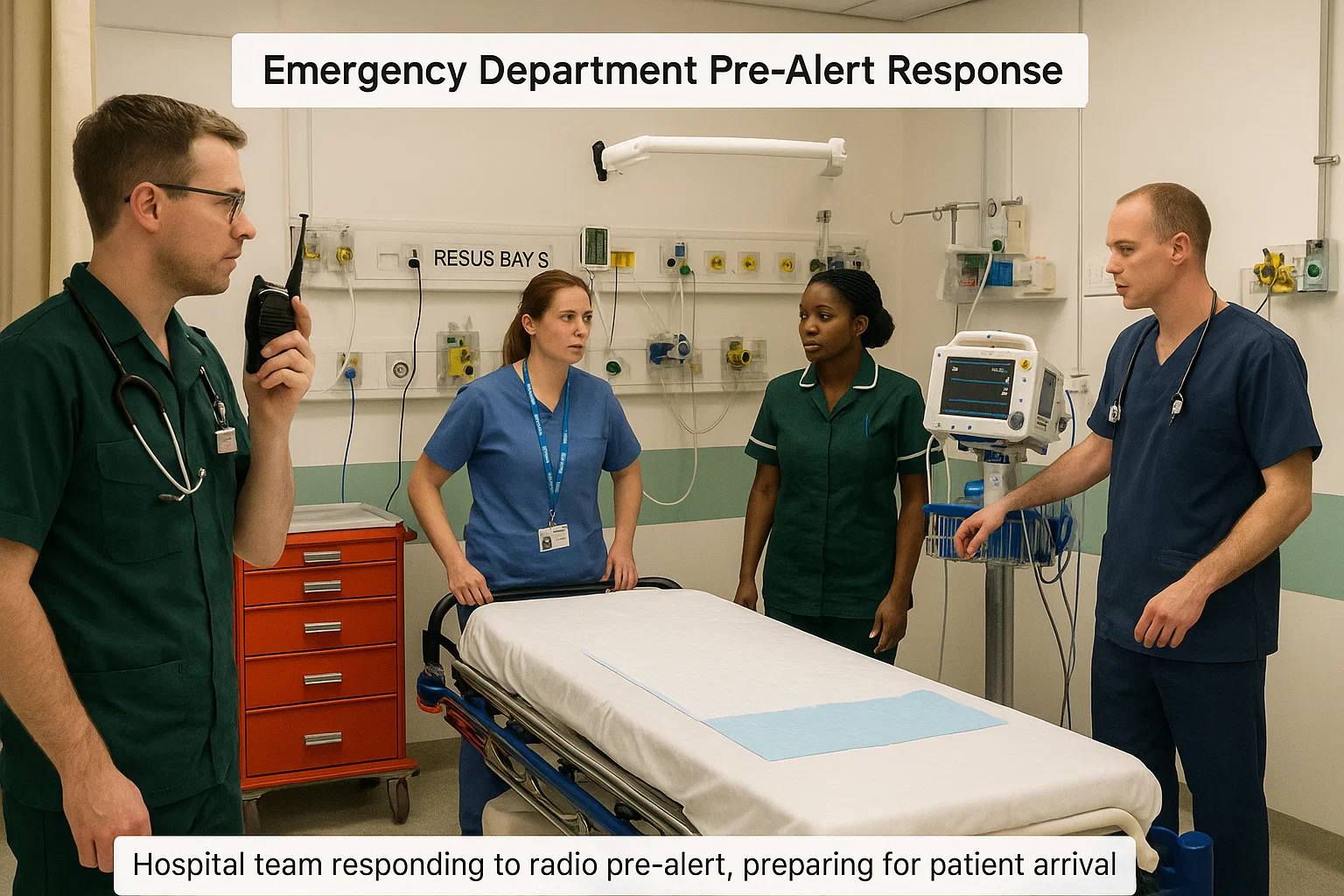
Inside the Emergency Department: Receiving the Call
From the hospital side, the nurse in charge or ED coordinator answers the radio channel or dedicated line. They document ATMIST data onto the handover whiteboard and alert consultants.
University Hospital Southampton (2025 Trial) found that when ED staff acknowledged every pre-alert verbally “Received, resus team ready” handover compliance rose from 81 to 94 percent.
Pro Tip Close the Loop:
Always wait for the hospital to repeat key details (age, ETA, chief complaint). No confirmation = no handover completed.
Coordinating With NHS Control Rooms
Control rooms serve as information hubs linking multiple hospitals. They log pre-alerts into Computer-Aided Dispatch (CAD) systems and monitor bed availability.
When a hospital diverts, control rooms relay updates via C3 CAD status code “D-Alert.” Crews must acknowledge within 60 seconds and confirm reroute.
Field note: During the 2024 Manchester Storm incident, rapid rerouting via radio pre-alerts saved nine critical care patients from divert delays averaging 30 minutes.
Case Study From Roadside to Resus in Seven Minutes
A London Ambulance crew responded to a 56-year-old male collapse outside a gym. ECG showed STEMI.
- 3 min on-scene: O₂ and aspirin administered.
- 4 min: Radio pre-alert sent using ATMIST.
- 10 min arrival: Cath lab ready.
Total “door-to-balloon” time = 27 min well under NICE target (90 min). The crew’s concise radio script enabled cardiology activation before arrival.
Documentation and Legal Traceability
All UK ambulance trusts require pre-alert details logged within the electronic Patient Care Record (ePCR). The time stamp serves as a legal indicator of handover attempt.
According to the Health and Social Care Act (Records Retention 2024), all pre-alert data must be retained for a minimum of 8 years.
If you use digital systems, verify that encryption meets NHS Cyber Essentials Plus 2024 standards.
Training and Continuous Improvement
NHS ambulance trusts deliver annual Handover and Pre-Alert Refresher modules covering:
- Simulation of multi-casualty radio loads.
- Digital EPR integration training.
- Pronunciation and stress communication techniques.
The College of Paramedics CPD 2025 Curriculum mandates at least 2 hours of communication simulation annually for EMTs and paramedics.
Future Direction: AI Assisted Pre-Alerts
By 2026, the NHS is piloting AI-driven speech-to-text transcription that records radio alerts directly into EPR logs, flagging missing ATMIST elements in real time. Early trials at St George’s Hospital, London showed a 17 percent reduction in omitted data points.
Automation will not replace paramedics’ judgment but it will make every second count.
Key Takeaways
- Stick to ATMIST for clarity and brevity.
- Make the call 5–10 minutes before arrival.
- Confirm receipt and document time.
- Use digital tools (Cresta, Cleric, C3 Cloud) for data integration.
- Always maintain a calm, professional tone under pressure.
FAQ Radio & Telephone Pre-Arrival Notifications (UK EMS)
Q1. Who is responsible for making the pre-alert call?
Usually the paramedic in charge or designated crew leader. Responsibility cannot be delegated to students without supervision.
Q2. What if radio coverage is poor?
Use mobile telephone as backup and notify control room. Log method used in ePCR.
Q3. Are digital alerts legally accepted as handover proof?
Yes, provided they are time-stamped within an approved NHS system and acknowledged by the receiving unit.
Q4. How long should a radio pre-alert last?
Aim for 30–45 seconds. Over 60 seconds reduces clarity and blocks other calls.
Q5. Can sensitive details (e.g., safeguarding) be shared over radio?
No. Use telephone or encrypted digital note via EPCR system.

Alex Smith, a seasoned medical technician with 15 years in ambulance services, writes crucial first-aid tips and emergency care insights on arescuer.com.
